Citation: Boffeli TJ, Tabatt JA. Minimally Invasive Early Operative Treatment of Progressive Foot and Ankle Deformity Associated With Charcot-Marie-Tooth Disease. The Journal of foot and ankle surgery. 2015;54(4):701-708.
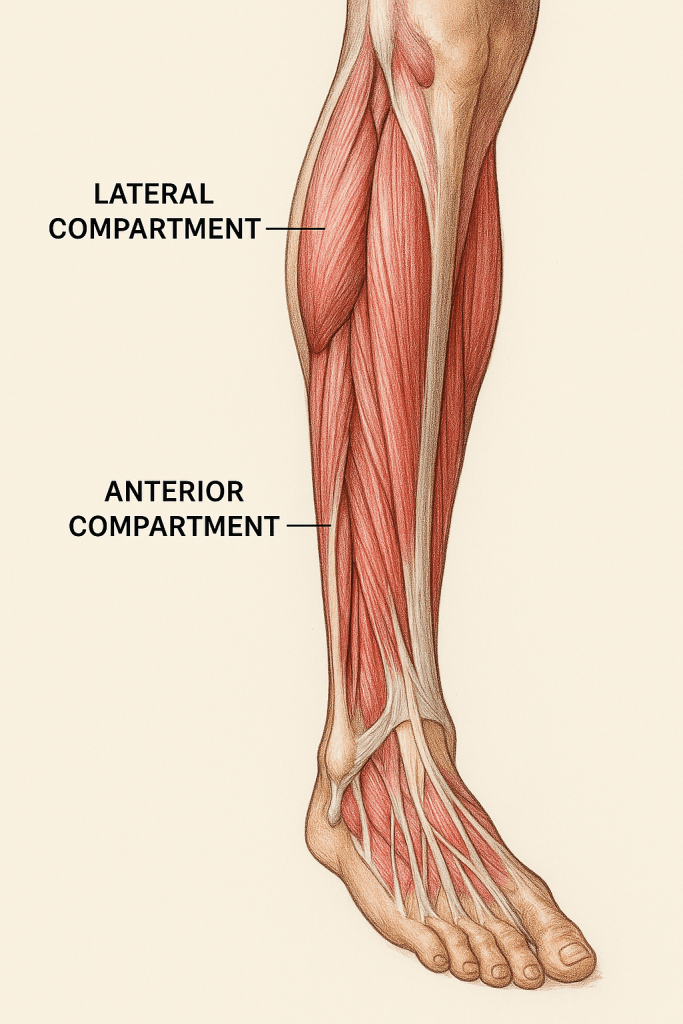
Charcot-Marie-Tooth disease is a neuromuscular disease that commonly affects the foot and leg. This disease follows a predictable pattern of muscle weakness typically affecting the intrinsic muscles of the foot as well as the anterior and lateral muscle groups, sparing the Peroneus Longus. When these muscle groups experience prolonged weakness, their antagonists overpower them, resulting in a classic cavus foot type. The loss of tibialis anterior leads to an overpull from EDL and EHL resulting in clawed digits. The loss of peroneus brevis and overcompensation from peroneus longus results in an adductovarus foot type. The calf muscles remain strong, resulting in severe equinus. As the muscle wasting progresses, the deformity proceeds into a rigid, nonreducible deformity. The idea presented in this article discusses the importance of early operative intervention before this rigidity is established and may allow for better results.
The techniques described in this article include an EHL transfer to the first metatarsal and EDL transfer to the midfoot. This should ideally improve ankle dorsiflexion and be performed before dysfunction of the tendons or before the toe deformity becomes too progressed. Additionally, the PL is transferred to the base of the fifth metatarsal. This allows for correction of the loss of PB and removes the plantarflexory force on the first metatarsal caused by overcompensation of the PL. TAL allows for further ankle dorsiflexion, and plantar fasciotomy to further improve first ray dorsiflexion. The authors discuss that Steindler stripping is not typically necessary when the deformity is not rigid.
Typical treatment for cavus foot, especially rigid foot deformities like those seen in late-stage CMT rely heavily upon extensive forefoot and hindfoot reconstruction. Soft tissue balancing does not provide enough correction in these types of patients, thus the authors propose for early soft-tissue correction in flexible patients, especially utilizing a minimally invasive technique. They cite an article (Tibrewal, 1989) which described a sample of patients who underwent soft-tissue procedures and no patient proceeded to a triple arthrodesis, the workhorse of the cavus foot recon, within the 14-year average follow-up. While the authors do understand the necessity for osseous reconstruction in late-stage progressed disease, they recommend early soft-tissue techniques which may help to slow or reduce eventual deformity.